SCORE COVID Seasonal Update Summer 2024

Written by Adam Tsuris and J. A. Sterling
SCORE = Socialist COVID-19 Organizing, Resistance, and Education
Introduction
The purpose of this seasonal update is to present the latest findings related to the ongoing COVID-19 pandemic. Everything here is based on peer-reviewed science. Conclusions and recommendations apply the precautionary principle.
The data emphasize the critical need for persistent vigilance to protect both personal and public health amid the evolving SARS-CoV-2 virus. Despite changes in the virus, transmission mechanisms and infection risks remain consistent, underscoring the importance of continued preventive measures such as high-quality respirators, air filtration, ventilation, and vaccination. The rise of more infectious and immune-evasive variants highlights the urgency of adapting strategies and staying informed. The shift towards privatized pandemic responses, particularly in testing and treatment, complicates access to resources and places more responsibility on individuals for their own protection. With weakened public health infrastructure and limited surveillance, it is crucial for individuals to proactively seek accurate information and timely medical interventions. Community support and regular updates are essential to navigating the ongoing COVID-19 threat, reinforcing the need for collective commitment to public health principles and personal safety measures.
Prompt Analysis
Risk of Long COVID/Post-Acute Sequelae of COVID-19
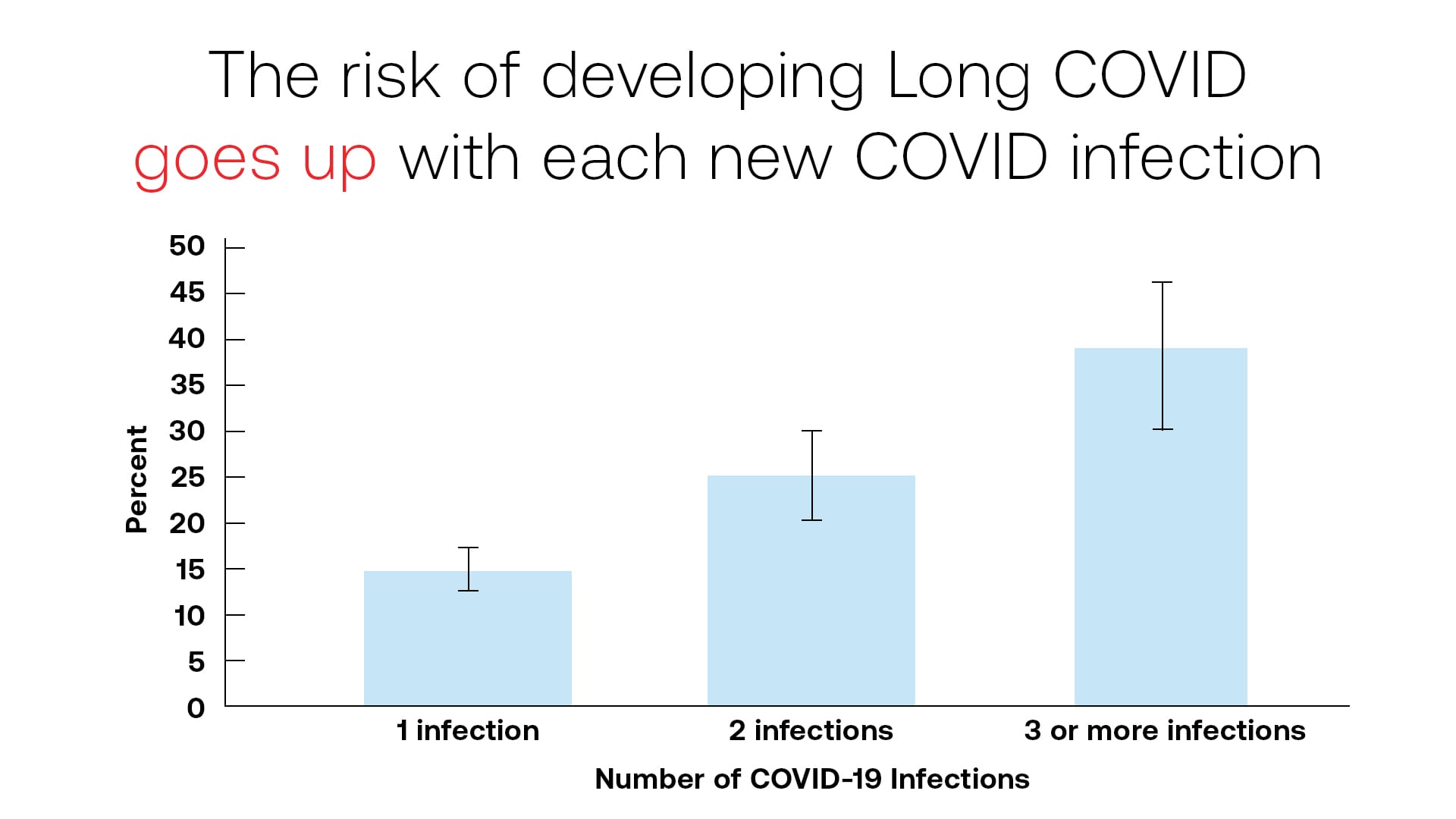
Many exposed to SARS-CoV-2 only have mild symptoms and 30%-60% of cases have none at all;[1] however, regardless of acute infection severity and regardless of COVID variant, each infection risks long-term symptoms, and each reinfection increases that risk[2]—the damage is cumulative. Some infections cause severe, long-lasting symptoms which do not dissipate over time.[3] Other infections result in increased vulnerability to post-COVID conditions, including but not limited to diabetes, blood clots, strokes, and heart failure.[4],[5] These conditions affect every part of the body to which blood and lymph flows (one’s vascular system) and range from mild to severe. According to the CDC[6] and Moderna,[7] the average risk of developing Long COVID/PASC is approximately 20% (1 in 5) and this risk only increases with each subsequent infection.[8] Age, pre-infection resilience, and physical capacity—in other words, how one “feels”—are not determinants of post-infection vulnerability, and the parts of the body affected are unpredictable. Children,[9],[10],[11] marathon runners, and rich celebrities are just as vulnerable to these long-term conditions as everyone else.
For those who experience this chronic illness, known as either Long COVID or PASC, a gradual improvement in symptoms may be experienced, but a plateau is common 6-12 months post-infection. Only 22% recover fully within a year.[12] Long-term recovery trajectories remain unknown. The data is proving this out, as disability rates have skyrocketed and continue to climb,[13],[14] whether looking at conservative economic estimates or as studied and reported by the USA Social Security Administration.
An alternate explanation for this rise in illness, disability, and death is the concept of “immunity debt,” that the general population is in poorer health now because, for the brief period of time when public health measures were adopted, they were not being infected by viruses as frequently as before. However, physiological science has proven the immune system is not like a muscle. It does not need to be exercised to remain strong—the opposite is true. Many cases can be analyzed to test the immunity debt hypothesis. One such example is recent pediatric influenza hospitalization data,[15] which confirms at a glance that naive immune systems are more resilient. A much larger sample size is evident if one compares the rise in poor health and mortality experienced in countries that took no public health measures[16],[17],[18] and within the population of children across the world who were born after public health measures were abandoned.[19] Based on the abundance of evidence, particularly the health outcomes of children born after public health measures were lifted, one can reasonably conclude that the cause of the rise in illness, disability, and death throughout society is not due to “immunity debt,”[20],[21] but rather due to the uncontrolled spread of the virus SARS-CoV-2,[22],[23],[24] which has been proven to cause illness, disability, and death, both directly[25] and via immune system dysregulation.[26],[27]
In addition to the known long-term effects of SARS-CoV-2 infection, the history of other pathogens indicates a high likelihood of other unknown post-acute sequelae arising in the future. HIV to AIDS takes an average of 12 years; Polio to post-Polio syndrome 15 years; HPV to cervical cancer can take decades; mono (Epstein-Barr Virus) to Multiple Sclerosis and other autoimmune conditions can take decades; Chicken Pox to Shingles, also decades. Acute HIV and acute Polio are brief, mild, flu-like illnesses. Scientists and doctors are currently encountering Long COVID caused by infections that resolved three years earlier.[28] There is also compelling evidence showing a link between SARS-CoV-2 infection and cancer.[29]
Currently, this is the limit of understanding of Long COVID/PASC. There is no cure at this time. The known risk of Long COVID/PASC on a per-infection basis has not meaningfully changed as new COVID variants have emerged, and the overall risk has increased due to the increased data availability concerning recovery,[30] reinfection, and the development of Long COVID/PASC.
Risk of Acute Infection
SARS-CoV-2 is a virus which causes a vascular infection (COVID-19) and which is transmitted primarily by a respiratory route. In other words, COVID spreads via one person breathing out and another person breathing that same air in. The majority of transmission occurs before symptoms appear.[31] Additionally, COVID can hang in the air for over 12 hours,[32] meaning that even an empty room is not necessarily a safe room (e.g. an empty exam room in a medical clinic, an empty aisle of a supermarket, or a public toilet). This has not changed as new COVID variants have emerged. Since the SARS-CoV-2 virus travels through and lingers in the air like smoke, indoor spaces have especially high potential for infection. However, it is important to understand that one can also easily be infected outdoors. There is overwhelming, documented evidence of outdoor transmission.[33],[34],[35],[36],[37]
The Relative Infectiousness (relative “Growth Advantage”) of dominant variants has only increased. In other words, risk due to wearing a low-quality mask, or a high-quality mask which is not fit-tested, or not masking outside, has increased. More precaution is needed now than was needed previously to avoid infection.[38],[39]
Even though the SARS-CoV-2 virus can survive for a long time in lab conditions, many studies suggest that it is not likely to spread by touching non-living surfaces on which the virus is deposited (fomite transmission).[40],[41],[42],[43],[44],[45] There is a growing body of evidence that glasses wear lowers the risk of COVID, at least for contact with gross droplets (e.g. being sneezed on); however, the significance remains unknown.[46]
There is a growing body of evidence for zoonosis (transmission from animals to humans)[47] and reverse zoonosis (transmission from humans to animals).[48] It is important to keep this in mind, both to keep yourself safe from your pets and to keep your pets safe from you. Cats, dogs, and rats frequently get infected by the virus and suffer from its effects, both in the acute phase and in the long term.[49],[50],[51],[52],[53]
Current Variant(s)
The most prevalent variants this season (April to August 2024) are descendants of the JN.1 lineage, which began its path to dominance in October 2023, by way of JN.1.11.1 (now called the KP lineage).[54],[55]
JN.1.11.1 has as its single most beneficial mutation a set of mutations that increase the binding strength to human ACE2 receptors, which are necessary for our metabolism and present throughout the body. Specifically, the S:F456L mutation which has been detected concurrently with S:L455F.[56] Variants with both S:456L and S:L455F mutations are the ones called the FLip variants.[57],[58],[59] S:F456L and S:L455F both greatly increase the affinity of the virus for ACE2 receptors. ACE2 receptors are the main way COVID enters cells (using the spike protein into ACE2 receptors like a key into a lock). In other words, they make it even easier for COVID to infect cells, and harder for one’s body to identify and clear the infection through antibodies that target the spike protein.
S:L455F also confers some immune escape. Immune escape does not just mean that the virus better evades the body’s protections but rather that the human immune system is not capable of mitigating the virus on its own without at least an updated vaccine. This challenge is compounded by the problem of Original Antigenic Sin (i.e. antigenic imprinting), where the immune system preferentially recalls previous virus variations against which it learned to defend itself and is incapable of adapting due to the very high, but not actually 100%, similarities with the current variant.
The most prevalent COVID-19 variants currently are the KP.3, KP.2, and LB.1 lineages.[60],[61] The KP.3 lineage is already outcompeting the other two and all variants in circulation. The KP.3.1.1 variant in particular is spreading particularly fast, showing a greatly increased infectivity and immunity-evasion compared to even the KP.3 variant from which it descended.[62],[63]
KP.3 and LB.1 seem to have their growth advantages because of two specific additional mutations (S:Q493E and S:Q183H, respectively).
KP.3 may have an advantage over LB.1 due to the S:V1104L mutation, which is thought to increase local stability. In the context of viral evolution, "local stability" refers to the resilience of a specific viral variant within a particular environment or population. This stability means that the variant can maintain its prevalence and functionality despite various selective pressures, such as immune responses, antiviral treatments, or competition with other variants. A virus with better local stability will have more favorable future viral evolution because local stability enables a virus to maintain its presence and propagate effectively within a given environment or host population.
None of these variants exhibit different symptoms compared to previous ones. For approximately the last year, the XBB/BA2.86/JN.1 era, the most common symptoms have been: fever, chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea.[64],[65],[66] If you, or anyone with whom you have shared air, develop any of these symptoms, you should consider testing.
It is worth noting that the median (not average) time between exposure and the presence of detectable infection (COVID Incubation Period) has reduced from 5 days to 3.75 days.[67] It is possible this is indicative of a trend in the direction of viral evolution. The data supporting this trend go through January 2023.
Proactive Considerations
Infection Rates
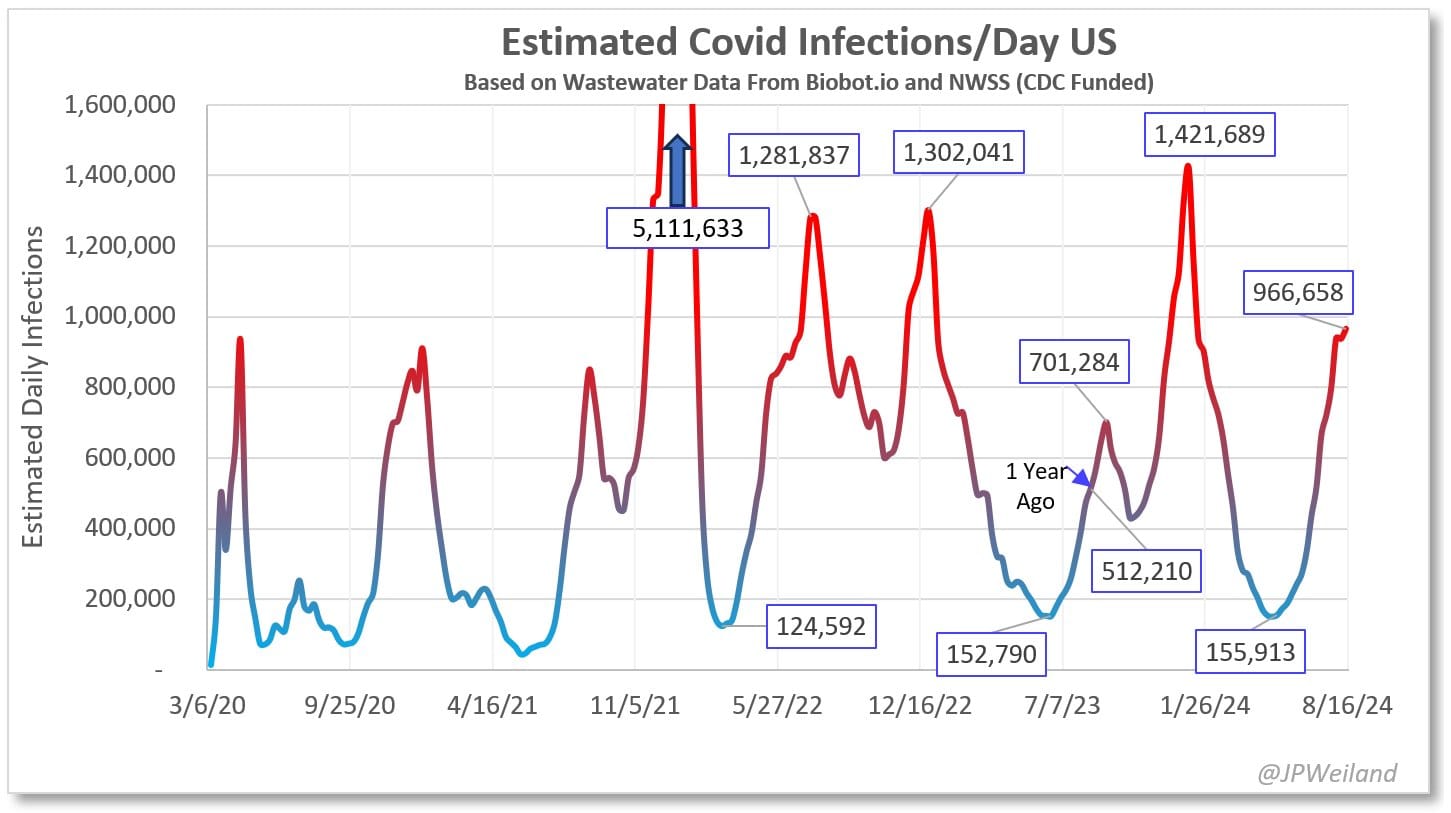
Wastewater data reveals that Summer 2024 has been an escalating COVID wave. On August 9th, it is estimated that there were over 1,000,000 new infections in The United States and that 1 in 33 Americans were experiencing active infections. The situation in Western and Southern states is particularly dire, with 1 in 22 and 1 in 25 people infected respectively and with case totals eclipsing the winter peak.
While the same safety measures are recommended regardless of if a wave is occurring or not, it is important to identify just how much danger one is in at any time for the purpose of scheduling necessary dental or medical care that might involve unmasking. Unfortunately, the danger is continuing to increase, since even case counts during troughs are at emergency levels—during the most recent trough in April 2024, the United States was still seeing nearly 300,000 new cases per day,[68] which is 91 times greater than the 3,300 daily case threshold cited by White House Chief Medical Advisor Dr. Anthony Fauci as necessary for gaining control of spread.[69] Additionally, in some locations, case counts in a trough have ended up being even higher than the peaks of previous waves. The case count for the trough between the current wave and the upcoming winter wave is projected to be 800,000.[70] This is not only 242 times greater than the threshold for “under control” but approaching the case count for the peak of the Delta wave.
Testing
As part of the Biden administration’s plan to privatize the response to the pandemic, the cost burden of testing has been shifted to the individual. Not only has the government’s free rapid test program been discontinued, but the free drive-thru PCR sites that were so common earlier in the pandemic have been dismantled. For most, getting a PCR test now involves making a doctor’s appointment, paying for the test out of pocket, and, consequently, a high risk of COVID exposure or spreading COVID due to the lack of infection control in medical settings.
The following infographic was posted by Twitter/X account @Clean_Air_Club_ and is shared here with its citations. The original post is available here (at the time of writing) and archived here. Citations include: [71],[72],[73],[74],[75],[76],[77] As stated earlier, over the last 4.5 years, the median (not average) time between exposure and the presence of detectable infection (COVID Incubation Period) has reduced from 5 days to 3.75 days.[78]
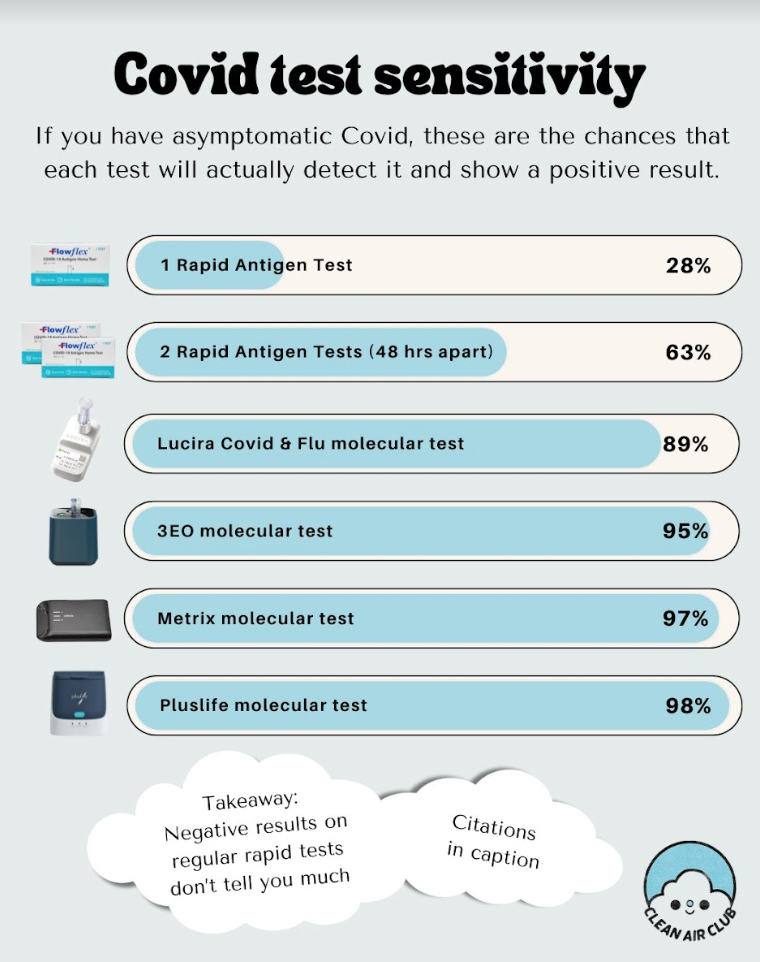
Rapid Antigen Tests (RATs) remain the least expensive but least accurate method of testing for COVID. The following caveats are extremely important for understanding RATs:
- A single positive result on a RAT means you have been infected and are contagious.
- A single negative result on a RAT, however, does not mean you do not have COVID. False negatives on RATs, especially when asymptomatic or presymptomatic, are extremely common, to the order of approximately 72%.[79] Even with symptomatic infections, it is common for people to consistently test negative several days after their symptoms begin.
In order to increase test accuracy, a combined mouth-throat-nose swab should be performed, because combined location swabbing results in detectable virus 1-2 days earlier.[80] The nose portion should be carried out by swabbing one’s nasal cavity instead of swabbing up one’s nostrils. This has been established as best practice ever since the original Omicron variant became dominant.[81] Please see a video demonstration here.
There are also a number of much more accurate but more expensive home molecular tests on the market. On top of the increased cost, these have a tendency to error out and unlike RATs can have a non-negligible false positive rate. However, these tests have an 89% to 97% chance of detecting an asymptomatic COVID infection.
The primary new development in testing this season is that there is now a new home molecular test (PlusLife) that not only has a 98% chance of detecting an asymptomatic COVID infection but also has an extremely low false negative and positive rate. Its primary improvement over prior tests in this range of sensitivity is a report of quantitative (graphical) results instead of a “yes/no” result (or “error”). For more information and extensive research, check the excellent community-made FAQ at https://virus.sucks/pluslife_en/.
Vaccination
Staying up to date on vaccinations remains an important tool in the toolbox. However, vaccination is not something that can be relied upon singularly for protection. Value vaccination like an airbag in a vehicle: something you absolutely want to have but never want to put to the test.
The vaccines currently available in the United States target the XBB.1.5 variant, a variant that is no longer in circulation and that is antigenically distinct from JN.1 and the currently dominant KP.3, KP.2, and LB.1 variants that descended from it.[82] While the current vaccine does still offer a level of protection from current variants in the acute phase against death, critical illness, hospitalization, and symptomatic infection:
-
it does not do so at a level that justifies abandoning other tools like masking, and[83]
-
the protection wanes rapidly with time, declining severely after 4 months.[84]
Similarly, no vaccine offers sufficient protection against Long COVID or PASC to justify unmasking.[85],[86],[87]
An updated vaccine is expected to become available in the autumn in the United States. After originally recommending that it target the JN.1 variant, the FDA is now recommending it target the KP.2 variant due to JN.1 having been pushed out of circulation.[88] Moderna and Pfizer are expected to have a KP.2 based vaccine ready, while Novavax is expected to have one based on JN.1. Neither variant is expected to be dominant when the vaccine becomes available.
Reactive Considerations
Prompt Response To Infection
Upon suspecting or confirming you have been infected, it is important to immediately isolate oneself from others so as not to infect them. Despite how transmissible SARS-CoV-2 is, it is possible to avoid in-home transmission through a combination of N95 masks, air purifiers, and ventilation. Some guidelines:
- The infected person should be isolated in a room with a window fan blowing OUT the window, with an air purifier running, and with any gaps in the door stuffed or sealed.
- The non-infected persons will avoid entering that room, run air purifiers, and have window fans blowing fresh air INTO their living space.
- Whenever the infected person has to leave the isolation room (i.e. to go to the bathroom), they should be wearing an N95. Ventilate the bathroom fully or wear an N95 if using the bathroom soon after the infected person has used it.
The more time that all parties can wear an N95, the less of a chance of transmission. More detailed information on how to prevent spread has been compiled by Clean Air Crew here.
Effective Mitigations
Paxlovid
Paxlovid is the most effective (and at this point, only) antiviral medication proven effective against COVID-19. It inhibits viral replication, thereby reducing acute infection severity, the risk of hospitalization, and the risk of death. Furthermore, it has been proven to reduce one’s chances of developing Long COVID.[89] If infected, it is vital to take Paxlovid if you are medically able regardless of perceived infection or symptom severity, and ideally as quickly as possible.
Paxlovid is typically issued as a 5 day course. Sometimes symptoms improve over those five days but then begin to return. This situation, often referred to as “Paxlovid rebound,” is not caused by Paxlovid, but instead by the 5 day course not being enough to clear the virus. A helpful analogy for “Paxlovid rebound” is stopping one’s antibiotic treatment at the sign of improved symptoms but before the infection is overcome. Paxlovid was originally intended to be taken as a 10 day course and is more effective that way,[90] and this is in fact the course that Dr. Fauci took when he was first infected.[91]
Unfortunately, it is not always easy to get a Paxlovid prescription in a timely manner (or at all). Many doctors caution patients that it is only beneficial in especially severe cases or in particularly at-risk populations, or that it causes rebounds or is not effective at all. Unfortunately, a doctor is very important to consult depending on the medications you take that may have harmful interactions with Paxlovid. If one’s doctor refuses to prescribe Paxlovid for an invalid reason (valid reasons being medications or conditions that are dangerous with Paxlovid), a prescription may be obtained through a telehealth service. Some states have their own Paxlovid telehealth lines, and there are several online private telehealth services as well, including Sesame Health, Dr. B, Push Health, and Plush Care.
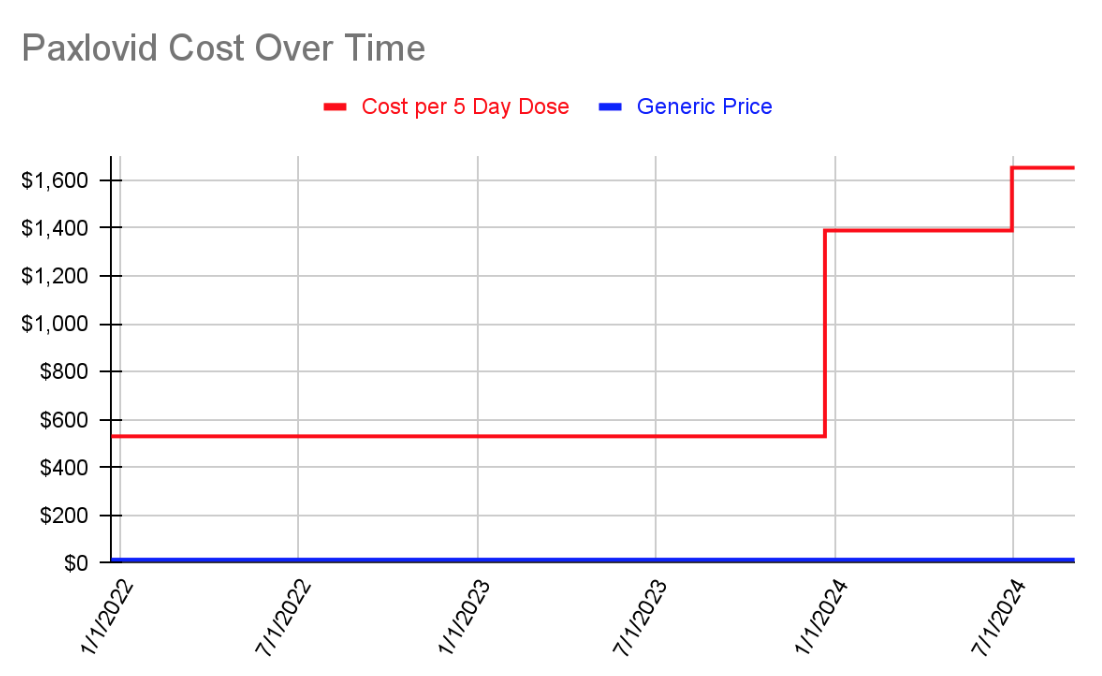
Prior to December 2023, the cost of Paxlovid was covered entirely by the US government. The cost has since been shifted to the individual and dramatically increased. The estimated generic cost of a 5 day course of Paxlovid is $15.08.[92] For the duration of time it was covered by the government, the price was set at $530.[93] When the government stopped covering it, the price increased to $1390[94] and then again to $1692 before insurance.[95]
Rest
Rest is absolutely essential after being infected—too much physical activity while infected or before one’s body has fully recovered increases the chances of developing Long COVID and PASC. This is a serious vascular disease that can damage every system in one’s body invisibly. At the very least, it is recommended to wait seven to ten days after being symptom free and testing negative before returning to exercise, but the more rest the better—three months is ideal.[96],[97] When finally trying to exercise again, it is important to do so very minimally and gradually, and stop immediately at the sign of any limitations, issues, or unnatural fatigue. A heart monitor should be worn as well.[98]
Metformin
Metformin—a common, inexpensive diabetes medication—may reduce one’s chances of developing Long COVID after infection. A promising study from earlier in the pandemic showed a 40% reduction in Long COVID,[99] and a new study has just been released showing a 42% reduction in Long COVID, a 3.6x reduction in viral load by day ten, a 58% reduction in the risk of hospitalization, and a 32% reduction in the risk of rebound.[100] It is something worth discussing with one’s doctor.
K12 Oral Probiotics
There is evidence that taking Streptococcus Salivarius K12 Oral Probiotics for at least two weeks can reduce the severity of one’s COVID infection.[101] These probiotics are available without a prescription and can be found online and at pharmacies.
Neosporin
There is new evidence that applying neomycin (OTC Neosporin) to the insides of one’s nostrils can help block infection.[102] It is important to understand that this is not a substitute for wearing a respirator—it is merely an extra layer of defense—and for a substantial number of people comes with the risk of allergic contact dermatitis and secondary dermatosis.[103]
Nasal Irrigation
On top of being a tool to use pre-exposure, nasal irrigation can be used post-exposure in order to help relieve symptoms and help one’s body clear the virus faster.
There is evidence that rinsing one’s nasal passages after a potential exposure can help prevent the virus from taking hold or possibly reduce the viral load one’s system is exposed to (and thereby possibly reduce the length and severity of illness).[104] One will need distilled or boiled water, saline packets, and either a neti pot or a squeeze bottle. More information including a detailed walkthrough has been shared by Clean Air Club on Twitter/X here, archived here.
Studies have shown (references indicated below) that over-the-counter Iota-Carrageenan, Hypromellose, Nitric Oxide, and Xylitol nasal sprays can reduce one’s chances of developing a COVID infection if exposed. Overall, though, the evidence can be summarized to say that doing some kind of nasal irrigation will result in some amount of risk reduction.
| Spray Type | Common Brands | Potential Risk Reduction |
| Iota-Carrageenan | FLO Travel, Betadine | 80% |
| Hypromellose | Taffix | 78% |
| Nitric Oxide | Enovid | 75% |
| Xylitol | Xlear | 62% |
Table References
Iota-Carrageenan[105],[106],[107],[108],[109],[110]
Hypromellose[111]
Nitric Oxide[112]
Xylitol[113]
In general, these sprays can be used both before and after a potential exposure. It is important to understand that these sprays are not a replacement for wearing a respirator and that the listed protection percentages are potential reductions in risk—nasal sprays should be viewed as a merely extra layer of protection, and one that is particularly important for unavoidable dangerous situations where unmasking is required (dental care, certain medical procedures, etc.). Discussion of the studies and results above has been shared on Twitter/X by Clean Air Club here, archived here.
Timeless Toolbox
Some items are not seasonal or in response to a known infection, and are instead persistent tools of pandemic self-defense.
Respirators
Wearing a respirator that fits you (whether a disposable N95 or an elastomeric with P100 filters) remains the single most effective way of protecting oneself from getting infected and infecting others, offering protection typically measured at 99.97%.
The best respirator is a respirator that fits you. In order to truly know if one’s respirator fits properly, a fit test must be performed. A fit test involves wearing a respirator, placing a hood over one’s head, spraying a fit test solution (bitrex or its sweet counterpart), and attempting to taste it while performing a set of motions.[114] This can be accomplished inexpensively at home by using a face mister and a garbage bag. If you cannot taste the solution, that means your respirator fits you properly. If you can taste the solution, that means your respirator either is not positioned correctly on your face and needs adjusting, or that it does not fit you and a different model is required.
For disposables, the 3M 9210+ Aura is a trusted respirator that is most likely to fit most faces. If the aura feels too small, the 3M 9105 Vflex or Dräger 1950 are good options. If the aura feels too large or if you are trying to find an N95 that fits children, the Trident P2 respirator may be a good fit.
For elastomerics, the 3M 7500 series (with 7093 P100 filters) and the 3M HF-800 Secure Click series (with D9093 P100) filters are excellent choices. The Flo Mask can be a great option for children ages 4 to 12 as well although many substitute the filter media.
Mask Bans
Throughout the world, anti-masking laws are starting to gain traction, while the lifting of pandemic emergency orders is by consequence reapplying existing, racist, anti-face covering laws. In the USA, with bipartisan support, North Carolina and Nassau County, New York have successfully put these into law,[115],[116] and New York (both city and state), Los Angeles, Chicago, and Philadelphia are considering similar legislation.[117] It is important to remember that it is still legal and essential to wear an N95 or elastomeric respirator for medical reasons–—namely, to prevent oneself from getting or spreading SARS-CoV-2–—but also that these laws contain language that will lead to increased harassment from police officers, business owners, and ordinary citizens.
The North Carolina and Nassau County laws that have passed provide a dangerous blueprint: in North Carolina, any person may demand someone remove their mask. In Nassau County, police officers are given the power to judge if one has a medical condition they deem worthy of wearing a mask.
For people living in areas with anti-mask legislation, it is recommended to obtain a doctor’s note that explains one’s respirator is being worn for medical purposes and to keep it on one’s person.
Air Purifiers
Air purifiers, both store-bought HEPA purifiers and homemade Corsi-Rosenthal Boxes (commonly referred to as Corsi Cubes), remain important and variant-proof tools in the fight against COVID-19. SARS-CoV-2 is airborne, and these devices remove the virus from the air.
If you decide to buy a HEPA air purifier, choose one that has an appropriate CADR (Clean Air Delivery Rate) while also factoring in other variables like cost and noise. CADR is reported in cubic feet of air filtered per minute. The higher the CADR, the faster the purifier can remove viruses from the air.
An appropriate CADR can be determined mathematically based on the size of the closed-off location you want to keep safe. Here is a link to one of many freely available ACH calculators to help with sizing. Due to the efficiency of air purifiers, it is always good to add a safety factor of 63% to the final result.
Consider a bare minimum ACH of 4, a reasonable minimum target of 6, and an ideal target 12 (or higher) for protecting oneself from being present with someone with an active COVID infection. Note that air purifiers, which require multiple passes to clean air regardless of their total CADR, will not be able to reliably prevent a physically present infectious person from infecting you so should not be understood as a way to safely remove one’s respirator indoors with someone else. Air purifiers are valuable for clearing a space that an infected (or possibly infected) person has been in, but now needs to be safe again or as one layer of mitigation in a location requiring vigilance (home with an infected cohabitant; a hotel room; etc.).
A Corsi-Rosenthal Box (also called a CR Box or Corsi Cube) can be an inexpensive alternative to buying a HEPA air purifier. It is a type of air purifier that can be made easily at home using a box fan, furnace filters rated MERV-13 or better, cardboard, and duct tape. Despite not using HEPA-rated filters, these purifiers can outperform many HEPA purifiers due to their capability to move large volumes of air quickly.
More information, including a comparison of various HEPA air purifiers and detailed instructions for assembling a Corsi Cube, can be found at: https://cleanaircrew.org/air-cleaners/.
Ultraviolet Light
Conceptually, ultraviolet sanitizers function like air filters, removing pathogens from the air. In the same way as an air purifier, this is a useful additional mitigation for making indoor spaces safe after potential exposure to the virus. At a population level, this tool would reduce spread significantly. However, no air cleaning technology will deactivate or remove the pathogen in the air in the time and space between you and a nearby individual having a conversation before you can breathe it.
The same as with air purifiers, UV will not be able to reliably prevent a physically present infectious person from infecting you so should not be understood as a way to safely remove one’s respirator indoors with someone else. The most reliable and most cost effective protection is a properly worn and fitted respirator.
There are also business interests operating in this space unscrupulously. People should be very wary of ultraviolet sanitizing lights unless they can personally analyze the spectrum and energy level each light emits. Incorrectly manufactured, advertised, purchased, and/or deployed lights can create hazardous ozone, damage skin and eyes, or simply do nothing to keep you safe.
Due to its higher complexity, significant cost, and limited benefit relative to other readily-available tools, it is recommended that many other layers of mitigation are maximized before training to understand and then implementing ultraviolet sanitizers as part of one’s pandemic self-defense.
Wastewater
Wastewater data is the most time-sensitive gauge of COVID transmission and is the most accurate monitoring method, though it is dependent on calibration. As illustrated by this chart from Santa Clara County Public Health, wastewater data reveals cases missed by testing.
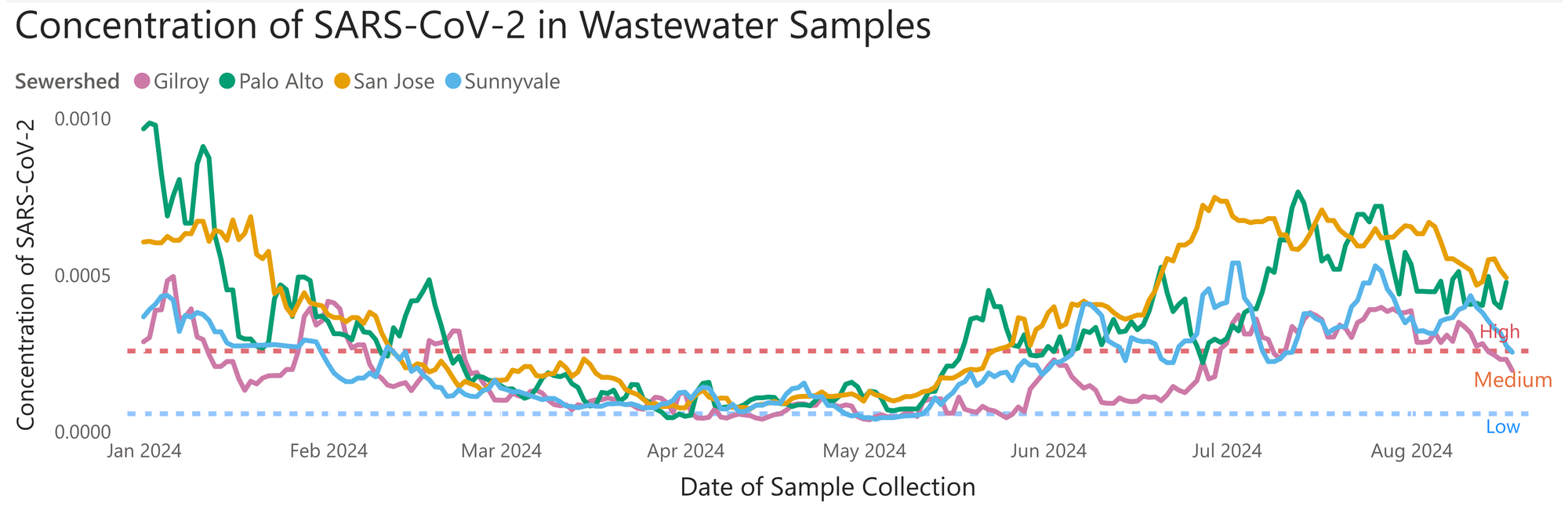
Our capacity to test for COVID-19 at the population level continues to be dismantled. The shift from PCR testing to unreported home rapid tests has concealed many infections, with few states having any mechanism for reporting personal RAT results. Having accurate wastewater data has only become more vital. Unfortunately, as pandemic and public health resources continue to be cut, it is becoming more difficult for the average person to find that information. Certain collection sites have unexpectedly stopped reporting data (often with no warning), and the CDC’s decision to end its contract with wastewater surveillance company Biobot to pursue a cheaper contract with Verily has cut the number of wastewater sites it tracks in half (from 400 to 200) and has left 10 states without any information at all.[118] For now, two excellent wastewater models to watch are Mike Hoerger’s Pandemic Mitigation Collaborative. JPWeiland’s model is also very helpful.
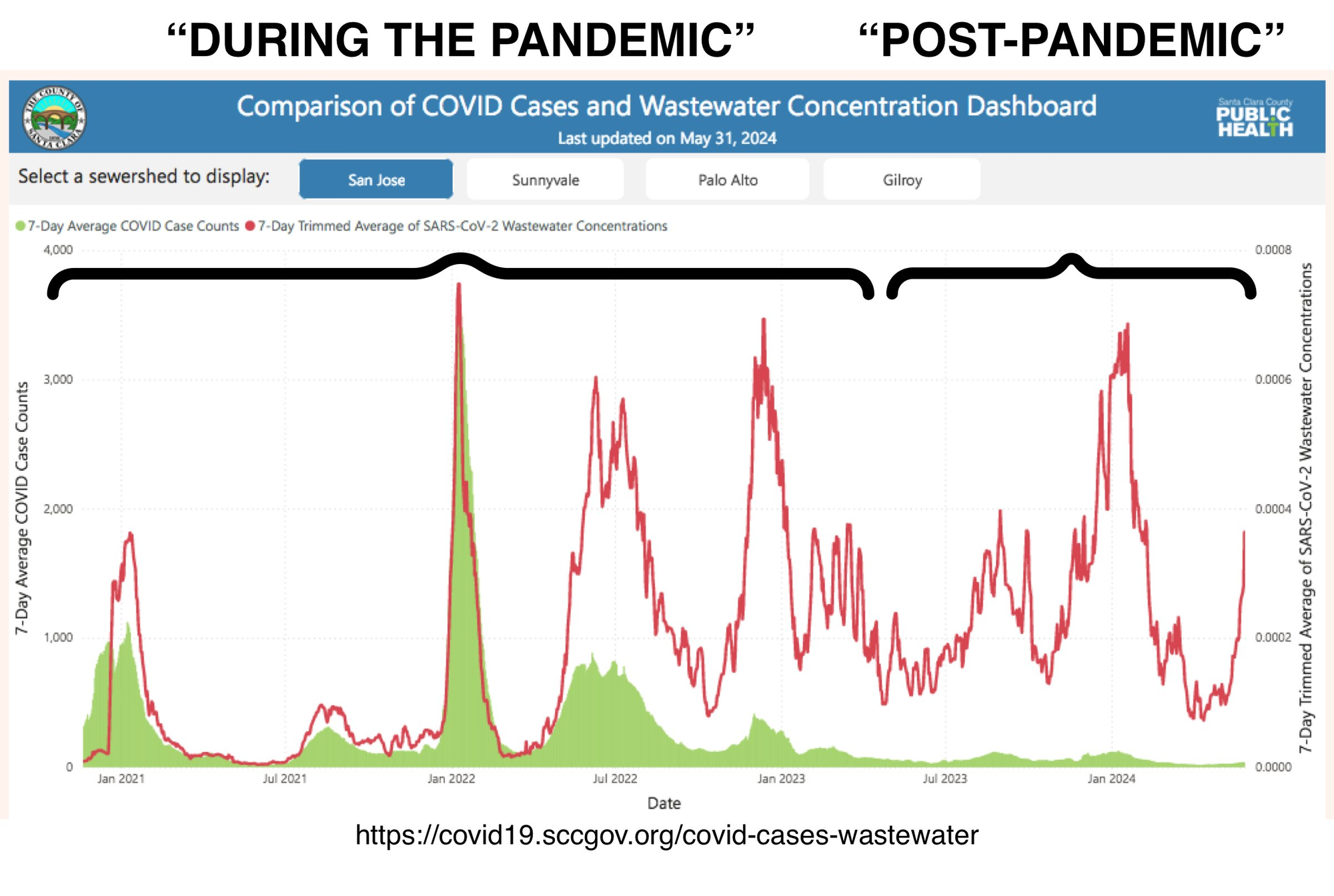
Wastewater data also illuminates the sociological production of the “end” of the pandemic. Consider Lee Altenberg’s fantastic comparison of “During” and “Post-Pandemic” wastewater levels based on the “Comparison of COVID Cases and Wastewater Concentration Dashboard” at the County of Santa Clara.[^120]
Travel Safety
While it is not recommended to travel during this ongoing pandemic, many people unfortunately are forced to do so by their employers or family obligations. Dynamic Zero will soon publish a COVID Safe Travel Tips article, so please check back with us!
Conclusion
The data continue to reinforce the importance of ongoing vigilance to safeguard our health and that of our loved ones. Despite the ongoing evolution of the SARS-CoV-2 virus, the fundamental mechanisms of transmission and the risks associated with infection remain largely unchanged. The cumulative impact of each infection and reinfection highlights the need for sustained preventive measures, including the use of high-quality respirators, air filtration, ventilation, and vaccination, even as new variants emerge. The increasing dominance of more infectious and immune-evasive variants underscores the urgency of staying informed and adapting our strategies accordingly.
The shift towards privatization and individualization of pandemic responses, particularly in the realm of testing and treatment, poses significant barriers to access to necessary resources. In parallel, as public health infrastructure faces regulatory capture and a dearth of surveillance data, undue responsibility is required of every individual for their own protection. This makes it all the more important for individuals to be proactive in seeking accurate information and timely medical interventions. Without community support and care, few have the capacity to face each day’s challenges in this arena. Regularly updated information and the publication of these updates is vital, and we seek to aid in that regard with this as the first in a regular series of updates.
Ultimately, the ongoing threat of COVID-19 and its long-term consequences necessitate a collective commitment to public health principles and personal protective measures. As we all navigate the complexities of this evolving pandemic, it is clear that maintaining a high level of awareness and precaution is essential to protect ourselves and our communities from the pervasive risks posed by SARS-CoV-2.
Notes
https://pandemicpatients.org/home/covid-19-resources/lc-pcc/ ↩︎
https://www.modernatx.com/en-US/media-center/all-media/blogs/long-covid-awareness-day-2024 ↩︎
https://www150.statcan.gc.ca/n1/pub/75-006-x/2023001/article/00015-eng.htm ↩︎
https://jamanetwork.com/journals/jama/fullarticle/2822770 ↩︎
https://publications.aap.org/pediatrics/article/153/3/e2023062570/196606/Postacute-Sequelae-of-SARS-CoV-2-in-Children ↩︎
https://www.abc.net.au/news/2024-06-16/children-with-long-covid-dismissed-doctors-myth-virus-harmless/103959078 ↩︎
https://threadreaderapp.com/thread/1601071762073997313.html ↩︎
https://www.barndiabetesfonden.se/globalassets/rapporten-om-typ-1-2024/bdf_rapport_t1d_2024_lr.pdf ↩︎
https://healthydebate.ca/2023/01/topic/debunking-myth-immunity-debt/ ↩︎
https://www.thegauntlet.news/p/nytimes-invents-increasingly-bizarre ↩︎
https://www.manager-magazin.de/hbm/long-covid-and-the-economy-there-is-money-in-prevention-a-54022db9-428f-41d7-b71c-3f9befa58b0e ↩︎
https://whn.global/covid-19-and-immune-dysregulation-a-summary-and-resource/ ↩︎
https://threadreaderapp.com/thread/1782302137684222267.html#google_vignette ↩︎
https://www.washingtonpost.com/health/2024/06/06/covid-cancer-increase-link/ ↩︎
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2820087 ↩︎
https://www.medscape.com/viewarticle/980195, https://pubmed.ncbi.nlm.nih.gov/35891214/ ↩︎
https://weekly.chinacdc.cn/en/article/doi/10.46234/ccdcw2022.209 ↩︎
https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.1153303/full ↩︎
https://www.thelancet.com/journals/lanepe/article/PIIS2666-7762(22)00030-8/fulltext ↩︎
https://www.sciencealert.com/virus-behind-covid-19-now-rampant-in-wild-animals-study-finds ↩︎
https://github.com/neherlab/SARS-CoV-2_variant-reports/blob/main/reports/variant_report_latest_draft.md ↩︎
https://www.idsociety.org/covid-19-real-time-learning-network/diagnostics/covid-19-variant-update/#/+/0/publishedDate_na_dt/desc/ ↩︎
https://jamanetwork.com/journals/jamaophthalmology/fullarticle/2795677 ↩︎
https://www.news-medical.net/news/20230403/Study-indicates-interspecies-transmission-of-SARS-CoV-2-between-humans-and-their-pets-occurs-regularly.aspx ↩︎
https://www.biorxiv.org/content/10.1101/2022.10.13.512053v1 ↩︎
https://web.archive.org/web/20231228065054/https://www.nytimes.com/2023/12/27/well/live/jn1-covid-variant.html ↩︎
https://www.cell.com/action/showPdf?pii=S0092-8674%2823%2901400-9 ↩︎
https://public.tableau.com/app/profile/raj.rajnarayanan/viz/USAVariantDB/VariantDashboard ↩︎
https://covid.cdc.gov/covid-data-tracker/#variant-proportions ↩︎
https://www.news-medical.net/news/20240722/Understanding-the-new-coronavirus-mutant-strain-KP311.aspx ↩︎
https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html ↩︎
https://publichealth.jhu.edu/2024/jn1-the-dominant-variant-in-the-covid-surge ↩︎
https://onlinelibrary.wiley.com/doi/full/10.1002/iid3.1323 ↩︎
https://www.cnbc.com/2021/11/16/dr-fauci-says-us-covid-cases-need-to-fall-below-10000-a-day-to-get-to-a-degree-of-normality.html ↩︎
https://josepheastman.substack.com/p/pathogen-update8-8-2024 ↩︎
Zhu et al., “Trial of the Pluslife SARS-CoV-2 Nucleic Acid Rapid Test Kit: Prospective Cohort Study” JMIR Public Health Surveill. 2023; 9: e48107. ↩︎
“Aptitude Metrix COVID-19 Test: Instructions for Use For Healthcare Providers” ↩︎
“Performance Evaluation of the Lucira COVID-19 + Flu Test” Note that PPA and NPA were used for the sensitivity and specificity stats above. ↩︎
Venekamp et. al. “Diagnostic accuracy of SARS-CoV-2 rapid antigen self-tests in asymptomatic individuals in the omicron period: a cross-sectional study.” 2023 ↩︎
Soni et. al. “Performance of Rapid Antigen Tests to Detect Symptomatic and Asymptomatic SARS-CoV-2 Infection” 2023 ↩︎
https://onlinelibrary.wiley.com/doi/full/10.1002/iid3.1323 ↩︎
https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(23)00101-5/fulltext ↩︎
https://www.ontariohealth.ca/sites/ontariohealth/files/2022-02/COVID-19RapidAntigenTests-HowtoCollectaSample.pdf ↩︎
https://www.cidrap.umn.edu/covid-19/xbb-booster-offers-protection-against-jn1-infections-hospital-cases-new-data-show ↩︎
https://www150.statcan.gc.ca/n1/pub/75-006-x/2023001/article/00015-eng.htm ↩︎
https://www.fda.gov/vaccines-blood-biologics/updated-covid-19-vaccines-use-united-states-beginning-fall-2024 ↩︎
https://medicine.wustl.edu/news/paxlovid-reduces-risk-of-long-term-health-problems-death-from-covid-19/ ↩︎
https://www.clinicaltrials.gov/study/NCT05047601?term=NCT05047601&rank=1&tab=results ↩︎
https://www.clinicaltrials.gov/study/NCT05047601?term=NCT05047601&rank=1&tab=results ↩︎
https://scholar.harvard.edu/files/melissabarber/files/estimated_cost-based_generic_prices_for_nirmatrelvir_ritonavir_paxlovid_january_2023_update.pdf ↩︎
https://www.reuters.com/business/healthcare-pharmaceuticals/pfizer-price-covid-19-drug-paxlovid-1400-five-day-course-wsj-2023-10-18/ ↩︎
ibid. ↩︎
https://www.jacc.org/doi/10.1016/j.jacc.2022.02.003 as discussed here: https://x.com/rajeevjayadevan/status/1719255835950690455 ↩︎
https://www.nebraskamed.com/COVID/how-and-when-to-start-exercising-again-after-covid-19 ↩︎
https://covid19.nih.gov/news-and-stories/can-diabetes-treatment-reduce-risk-long-covid ↩︎
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae159/7660393 ↩︎
https://mrmjournal.biomedcentral.com/articles/10.1186/2049-6958-9-57 ↩︎
https://www.researchgate.net/publication/353595904_Antiviral_Activity_of_Carrageenans_and_Processing_Implications ↩︎
https://www.respiratorytherapy.ca/pdf/RT-18-2-Spring-2023-R17-web.pdf ↩︎
https://multimedia.3m.com/mws/media/811473O/3m-qualitative-fit-testing-poster.pdf ↩︎
https://www.ncleg.gov/Sessions/2023/Bills/House/PDF/H237v6.pdf ↩︎
https://www.forbes.com/sites/judystone/2024/07/10/mask-bans-grow-threatening-public-health-and-immunocompromised-people/ ↩︎
https://prismreports.org/2024/08/06/covid-data-tracking-disappears ↩︎